Preventing HAIs with CLO₂ – Safer Hospitals, Smarter ESG Compliance
🏥 Hospital-Acquired Infections (HAIs): A Billion-Dollar Challenge
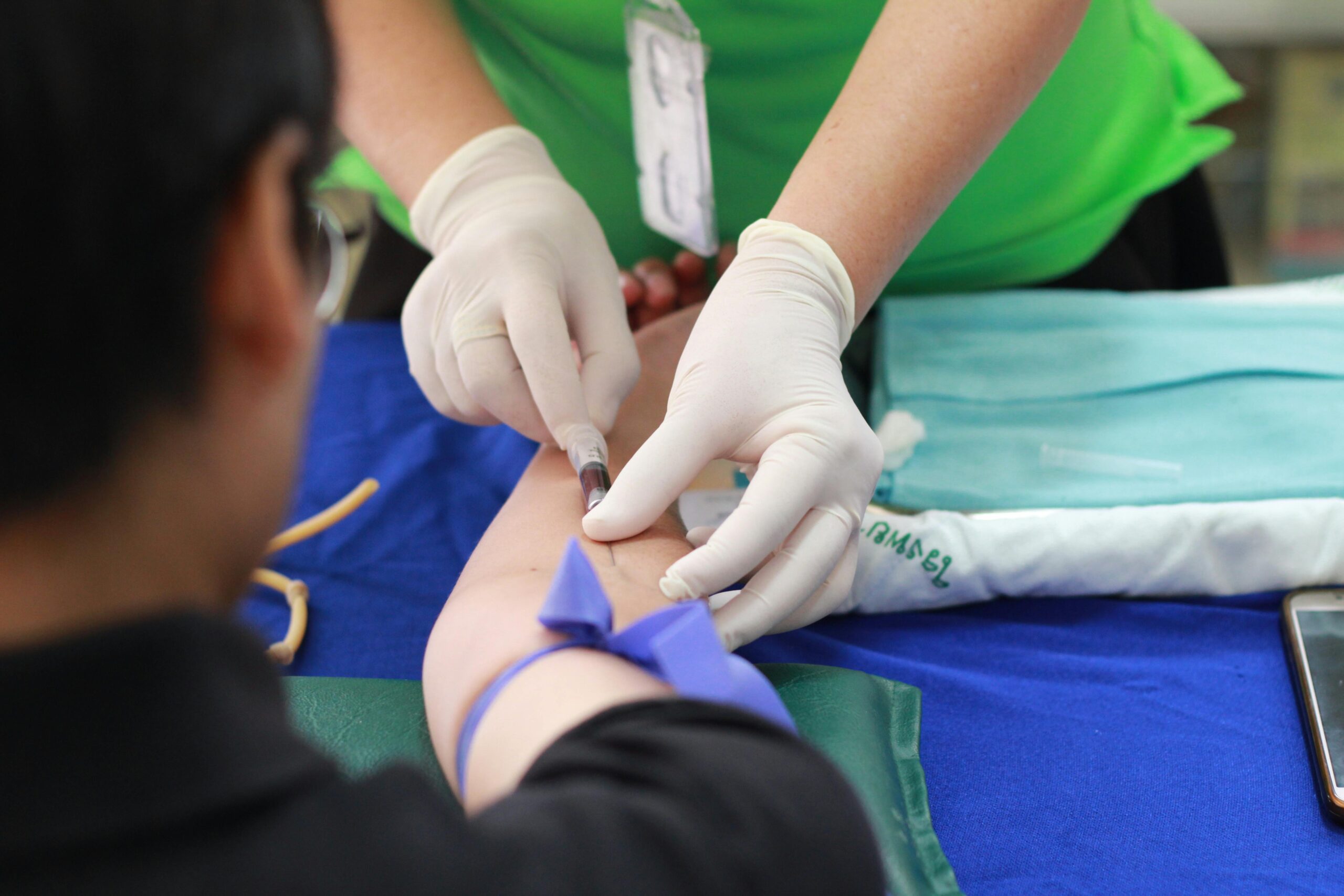
Every year, hospital-acquired infections (HAIs) silently claim thousands of lives and cost the healthcare system billions of dollars. From surgical site infections to deadly bloodstream pathogens, these infections are not just statistics—they are lives lost, recoveries prolonged, and reputations jeopardized.
Healthcare facilities are under relentless scrutiny: regulators demand compliance, insurers tighten coverage, and patients expect hospitals to be safe. Yet, even with standard infection control protocols in place, gaps remain—and every unprotected surface, every missed pathogen is a risk your hospital cannot afford.
The question is no longer if your facility will face these challenges—it’s when—and the decisions you make today can mean the difference between preventable outbreaks and lives saved.
 📊 HAI Statistics
📊 HAI Statistics
-
Prevalence: On any given day, about one in 31 hospital patients has at least one healthcare-associated infection.
-
Surgical Site Infections (SSIs): In 2023, there was a 2% increase in the standardized infection ratio (SIR) related to all National Healthcare Safety Network (NHSN) operative procedure categories combined compared to the previous year.
-
Catheter-Associated Urinary Tract Infections (CAUTIs): In 2023, 17,370 CAUTIs were reported across 3,774 general acute care hospitals.
-
Central Line-Associated Bloodstream Infections (CLABSIs): Data on CLABSI rates can be found in the CDC's HAI Progress Reports.
-
Methicillin-Resistant Staphylococcus aureus (MRSA) Bloodstream Infections: Information on MRSA bloodstream infections is available in the CDC's HAI Progress Reports.
-
Clostridioides difficile (C. difficile) Infections: Data on C. difficile infections can be found in the CDC's HAI Progress Reports.
🧼 Current Infection Control Standards
The Centers for Disease Control and Prevention (CDC) provides guidelines for infection control in healthcare settings. Key components include:
-
Standard Precautions: These are infection prevention practices that apply to all patients, regardless of their diagnosis or presumed infection status. They include hand hygiene, use of personal protective equipment (PPE), safe injection practices, and environmental cleaning.
-
Core Infection Prevention and Control Practices: These practices are designed to reduce the risk of healthcare-associated infections and include education and training of healthcare personnel, injection and medication safety, and the use of appropriate personal protective equipment.
-
Environmental Infection Control: Recommendations for environmental cleaning and disinfection in healthcare facilities to prevent the spread of infections.
⚠️ Why Current Standards May Be Falling Short
Despite the implementation of these standards, several factors contribute to the persistence of HAIs:
-
Antimicrobial Resistance: The overuse and misuse of antibiotics have led to the development of resistant pathogens, making infections more difficult to treat.
-
Inadequate Environmental Cleaning: Traditional cleaning methods may not effectively eliminate all pathogens, especially in high-risk areas.
-
Staffing Challenges: High turnover rates and insufficient training can lead to lapses in infection control practices.
-
Increased Patient Acuity: More complex patient conditions can increase the risk of infections.
Enter Chlorine Dioxide (CLO₂): Science-Backed Protection
Chlorine dioxide isn’t just another disinfectant—it’s a precision tool for hospitals. Here’s how it specifically supports healthcare organizations and enhances infection control where existing standards sometimes fall short:
1️⃣ High-Touch Surfaces
-
Problem: Door handles, bed rails, light switches, and nurse stations are notorious for harboring pathogens. Even with standard cleaning protocols, these areas can remain contaminated between cleanings.
-
CLO₂ Advantage: Its rapid action kills bacteria, viruses, and fungi within minutes, providing continuous protection in high-traffic areas. Hospitals can drastically reduce surface contamination, lowering the risk of HAIs.
2️⃣ Medical Equipment
-
Problem: Reusable medical devices (like stethoscopes, blood pressure cuffs, and surgical tools) are often vectors for infection. Traditional disinfectants may leave residues or require long contact times, making them impractical for fast-paced clinical environments.
-
CLO₂ Advantage: CLO₂ disinfects effectively with shorter dwell times and leaves no harmful residue, ensuring medical equipment is both safe and ready for immediate use—critical in operating rooms and ICUs.
3️⃣ Critical Care and Isolation Areas
-
Problem: ICU and immunocompromised patient units are high-risk zones. Airborne pathogens and surface microbes can spread rapidly, and conventional cleaning may miss microscopic reservoirs.
-
CLO₂ Advantage: Chlorine dioxide gas or solution can penetrate hard-to-reach areas, including air-handling systems and tight crevices, reducing microbial load in environments where vulnerable patients are at greatest risk.
4️⃣ Water Systems and Biofilm Control
-
Problem: Hospital plumbing systems and cooling towers can harbor biofilms, which are resistant to many disinfectants and can cause outbreaks (e.g., Legionella).
-
CLO₂ Advantage: CLO₂ is highly effective against biofilms, keeping water systems safer for both patients and staff, while preventing costly outbreaks that traditional disinfectants often fail to control.
5️⃣ Gap-Filling Where Standards Are Falling Short
 Even with CDC-recommended protocols, hospitals still struggle with:
Even with CDC-recommended protocols, hospitals still struggle with:
-
Missed micro-contaminated areas due to manual cleaning limitations
-
Pathogen resistance to traditional chemical disinfectants
-
Time constraints for repeated cleaning in high-traffic zones
CLO₂ fills these gaps by:
-
Offering broad-spectrum, rapid disinfection with minimal labor
-
Reaching areas standard cleaning cannot, including airborne pathogens and biofilms
-
Being eco-friendly and non-toxic, supporting staff and patient safety while reducing chemical exposure
🌱 ESG and Compliance Goals Aligned
Healthcare organizations are increasingly measured on ESG standards. CLO₂ supports these goals by:
-
Reducing chemical waste compared to traditional disinfectants
-
Lowering environmental toxicity
-
Maintaining regulatory compliance for infection control
-
Supporting staff and patient safety with a non-toxic alternative
🏥 Strict Current ESG Standards for Healthcare Organizations
Healthcare providers are under intense scrutiny to meet ESG standards, which encompass:
-
Environmental Impact: Reducing greenhouse gas emissions, energy consumption, and waste generation.
-
Social Responsibility: Ensuring equitable access to care, promoting patient safety, and fostering a diverse and inclusive workforce.
-
Governance: Upholding ethical standards, transparency, and accountability in operations and decision-making.
These standards are enforced through various regulations and reporting requirements, such as the Corporate Sustainability Reporting Directive (CSRD) in Europe and proposed climate disclosure requirements from the U.S. Securities and Exchange Commission (SEC) .
 ⚠️ Challenges in Meeting ESG Standards
⚠️ Challenges in Meeting ESG Standards
Hospitals face several challenges in achieving ESG compliance:
-
Complex Regulatory Landscape: Navigating diverse and evolving regulations across regions can be overwhelming.
-
Resource Constraints: Limited budgets and staffing can hinder the implementation of comprehensive ESG initiatives.
-
Data Management: Collecting, analyzing, and reporting ESG data accurately requires robust systems and processes.
-
Stakeholder Expectations: Balancing the demands of patients, regulators, and investors can be challenging.
📅 Frequency of ESG Audits and Potential Fines
Hospitals are subject to regular audits to assess ESG compliance:
-
Internal Audits: Conducted periodically to evaluate adherence to internal policies and procedures.
-
External Audits: Performed by regulatory bodies or third-party organizations to ensure compliance with legal and industry standards.
Non-compliance can result in:
-
Fines and Penalties: Regulatory bodies may impose financial penalties for violations.
-
Reputational Damage: Negative publicity can erode public trust and patient confidence.
-
Legal Consequences: In severe cases, legal actions may be taken against the organization .
🌿 How CLO₂ Helps Exceed ESG Expectations
Implementing CLO₂ in healthcare settings offers several benefits:
-
Environmental Impact: CLO₂ is effective in reducing chemical waste and lowering environmental toxicity compared to traditional disinfectants.
-
Regulatory Compliance: CLO₂'s efficacy supports infection control standards, aiding in meeting regulatory requirements.
-
Social Responsibility: By providing a non-toxic alternative, CLO₂ enhances staff and patient safety.
-
Governance: Demonstrating a commitment to sustainable practices can improve transparency and accountability.
By integrating CLO₂ into cleaning protocols, healthcare organizations can not only meet but exceed ESG standards, positioning themselves as leaders in sustainability and patient care.
🔹 Partnering with Synergy Green Clean and Envirotab: Your Strategic Advantage in Infection Control
In today’s healthcare environment, every infection avoided is a life saved—and every outbreak prevented is a financial win measured in millions. At Synergy, we don’t just provide cleaning products; we deliver science-backed, results-driven solutions that help hospitals reduce healthcare-acquired infections, protect vulnerable patients, and ensure staff safety.
CLO₂ isn’t a “nice-to-have” addition—it’s a strategic tool for hospitals that want to stay ahead of regulatory pressures, ESG mandates, and operational risks. Unlike traditional disinfectants that leave gaps in protection, CLO₂ provides broad-spectrum, rapid action, penetrates areas standard cleaning can’t reach, and reduces chemical waste—all while maintaining a safe, sustainable environment.
Choosing Synergy means choosing a partner who understands that infection control is not just compliance—it’s a competitive advantage. Protect your patients, safeguard your staff, enhance your ESG profile, and secure your facility’s reputation with a solution trusted by science.
CTA:
💧 Take the next step toward safer, smarter healthcare.
Explore our hospital-grade CLO₂ solutions and discover how Synergy can help your facility exceed infection control standards, achieve ESG goals, and redefine patient safety.
✅ Bottom Line for Hospitals:
Integrating CLO₂ into routine cleaning and disinfection programs doesn’t replace current standards—it enhances and strengthens them, giving healthcare organizations a science-backed advantage in infection prevention, ESG compliance, and patient safety.

🏥 FAQ: Hospital-Acquired Infections (HAIs) & Prevention
Q: What exactly are Hospital-Acquired Infections (HAIs)?
A: HAIs are infections patients contract while receiving medical treatment in a hospital or healthcare facility. They often involve bacteria, fungi, or viruses that thrive in clinical settings.
Q: How serious are HAIs?
A: Extremely. HAIs cause thousands of preventable deaths annually and cost the U.S. healthcare system billions of dollars. They also extend hospital stays and increase readmission rates.
Q: Which infections are most common in hospitals?
A: Surgical site infections, respiratory infections, bloodstream infections, and urinary tract infections rank among the most frequent.
Q: Why are HAIs such a major concern for hospitals?
A: Beyond the human cost, HAIs bring regulatory fines, lawsuits, and damaged reputations—making infection prevention a financial and ethical priority.
Q: Aren’t hospitals already disinfecting regularly?
A: Yes, but many traditional disinfectants fall short against biofilms, resistant pathogens, and hidden contamination hotspots.
Q: What role does chlorine dioxide (ClO₂) play in prevention?
A: ClO₂ is a powerful, eco-friendly disinfectant that penetrates biofilms, kills pathogens at the source, and works across surfaces and air without leaving toxic residues.
Q: Is ClO₂ safer than bleach or harsh chemicals?
A: Absolutely. Unlike bleach, ClO₂ breaks down into salt and water, leaving no harmful byproducts—making it safer for patients, staff, and sensitive equipment.
Q: Can ClO₂ help reduce costs for hospitals?
A: Yes. By preventing infections and reducing outbreaks, ClO₂ lowers patient readmissions, saves on extended care costs, and protects hospitals from regulatory penalties.
Q: How quickly does ClO₂ work?
A: In minutes. ClO₂ rapidly eliminates bacteria, viruses, and spores—even those resistant to conventional disinfectants.
Q: How can hospitals adopt ClO₂ solutions effectively?
A: Partnering with trusted providers ensures EPA-compliant ClO₂ protocols for room treatments, surface disinfection, and air quality control—delivering measurable reductions in HAIs.

 ⚠️ Challenges in Meeting ESG Standards
⚠️ Challenges in Meeting ESG Standards